The pandemic era re-shaped consumers’ views on food as an input for health across all dimensions. We look back with affection for our local grocery stores and pharmacies which played leading roles as first responders f0r our health and, quite literally, the basic needs at the base of our personal hierarchies the way Maslow conceived them.
As I tracked home-bound consumers’ behaviors from the start of COVID-19 in March 2020, I hunted-and-gathered data from Nielsen, Acosta, Circana, Gallup, Harris, and other sources of consumers @ retail. The DIY food-health concept, coined by Nielsen, was the build-up of our “pandemic pantries.”
Thus, food became a go-to for consumers seeking all manners of health, medical care, and well-being, from head (mental health) to toe (athleticism and resilience for those healthy walks outdoors).
We are now in our post-pandemic pantry modes. That growing life-flow, as consumers grew their value for food-as-medicine (broadly defined) is discussed in a new analysis from Deloitte, noting that Consumers want to eat their way to better health. Then asking, “How can health and business leaders help?” from Deloitte.

This analysis comes out of survey research Deloitte fielded in July 2024 among 2,014 U.S. consumers ages 18 and over.
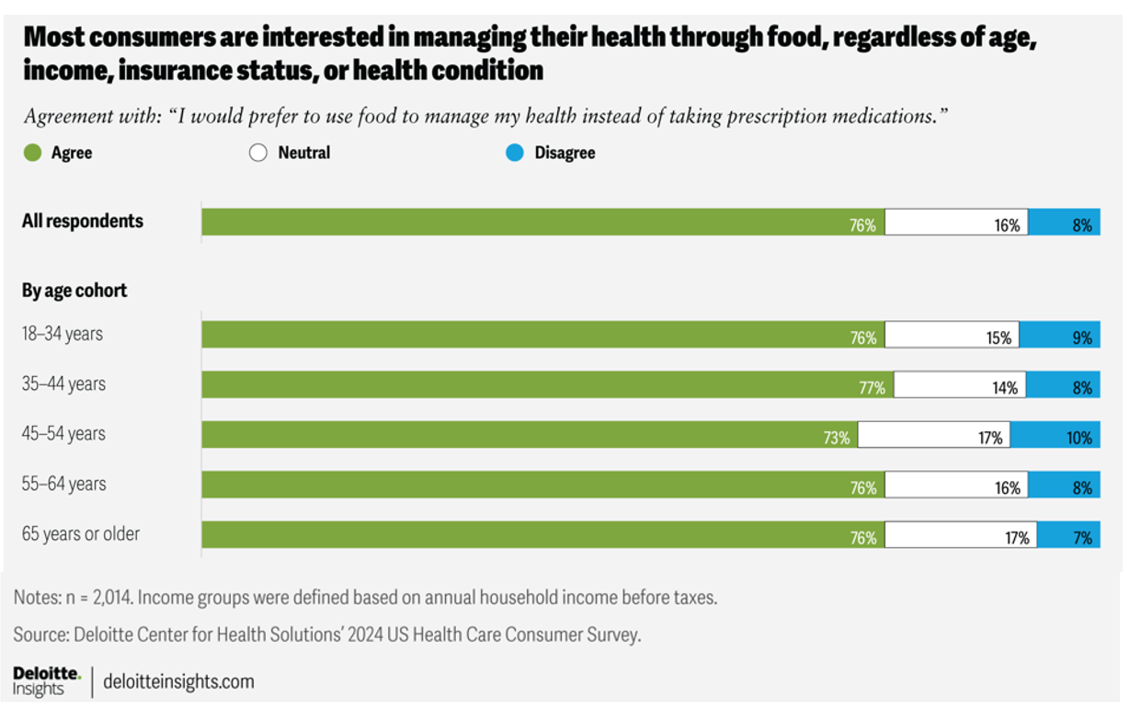
Overall, 3 in 4 U.S. adults are interested in managing their health through food.
It’s fascinating to see this sentiment is pretty equal across every demographic Deloitte assessed in the study: by age group, by income break, by insurance status, and by diagnosed chronic disease status.
Across all of these differences, we find most people embracing food as a health input and substitute for prescription medications.

By age: there is little variation from the 76% of consumers overall who would prefer to use food to manage health instead of prescribed meds.
Note that this true for 76% of the oldest age cohort of 65+ as it is for the youngest consumers ages 18-34 and those 55-64 years of age.

By income, too, there is little difference in the preference for food-as-medicine among households earning under $50K compared with those earning >$50K.
Similarly, for those consumers with health insurance compared with those who are uninsured, it’s still 3 in 4 people keen on food-as-medicine.
The biggest delta is seen among people diagnosed with chronic disease — somewhat fewer keen on food replacing prescribed medicines — versus people without chronic disease — with a 9-point difference among those dealing with a condition condition (73%) versus those with no chronic disease (82%).
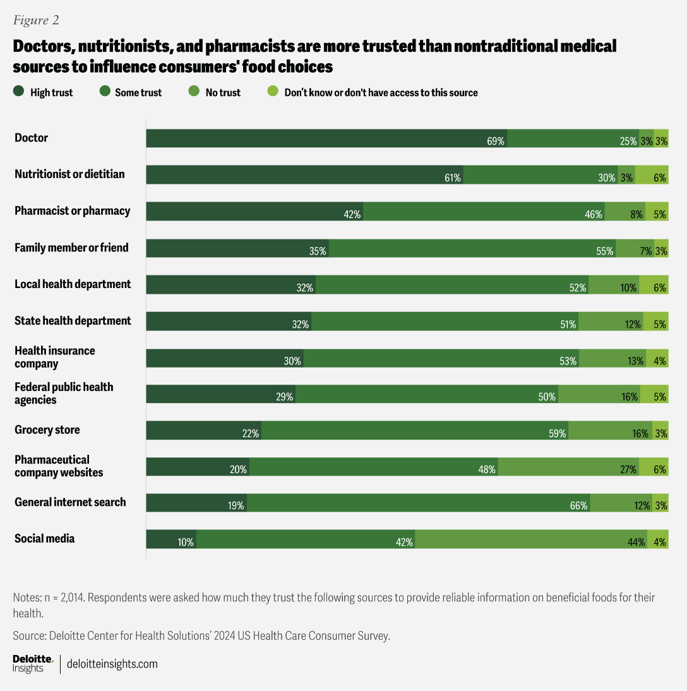
Health Populi’s Hot Points: In our era of mis-trust and grievance in and outside of the health care ecosystem, we must attend to the issue of messengers and trust when it comes to our demand for food-as-medicine.
Doctors rank top as most-trusted to influence consumers’ food choices, followed by nutritionists and dietitians,
Pharmacists and the pharmacies in which they work rank third, roughly tied with family members and friends in terms of net-trust for advice and influence on food choices.
The local and State health departments, and health insurance companies, rank next in the roster of trust-equity for food influence on our health.
I pointed to the grocery store as a health destination, curated during the coronavirus pandemic. We see grocers ranking lower for “high trust” than doctors or nutritionists, but “some trust” nets the trust as influencer up to near highs with that pharmacist or pharmacy.
Consider, then, the importance of the grocery store with co-located pharmacy and nutritionist on-board with the enterprise as a community trusted touch-point in the food-as-medicine supply side for consumers keen to add more healthy food inputs into their personal health ecosystems. As we continue to expand our definition of “retail health,” these trust touchpoints in peoples’ local communities can play important roles in moving care closer to people, their values and sense of value. Collaborations will be key to rebuilding trust and access in these times of possible food insecurity and health access eroding (e.g., SNAP benefit reductions, rural health access, etc.). That Deloitte’s lens on this topic focuses on “how can health and business leaders help?” more than hints at their understanding that it will take a village to rebuild public health and health citizenship.
I’ll be visiting this concept working with a client next week on how to expand consumers’ trust in the value of vaccinations, so collaborations that build/re-build trust in public and personal health are on my mind. Stay tuned for more on that — with appreciation to Deloitte for this lightbulb moment.