Health care costs will increase, overall, as much as 10% in 2026, the consensus of several health benefit analysts inform us. And, “workers to bear brunt of health cost increases in 2026,” reads today’s Axios headline on the topic, weaving together several studies from the Business Group on Health, Mercer, and the International Foundation of Employee Benefit Plans.

A kay cost-contributor cited in all of these health cost forecasts is the prescription drug line item: specialty drug prices, and specifically the costs of GLP-1 medicines and cancer therapies.
One strategy gaining fast-traction on both the supply and demand side of prescription drugs in the U.S. is direct-to-consumer/direct-to-patient programs that cut out “middle-men:” PBMs, formularies, and other intermediaries processing drug claims and access between prescribing clinicians and the patients who ultimately pay some portion or 100% out-of-pocket for medicines.
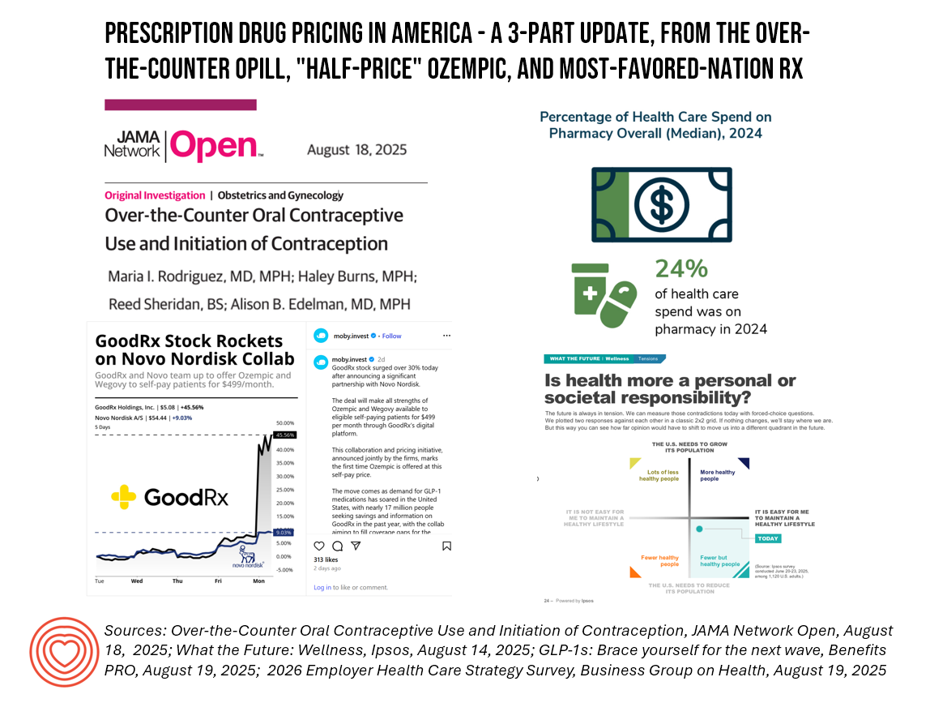
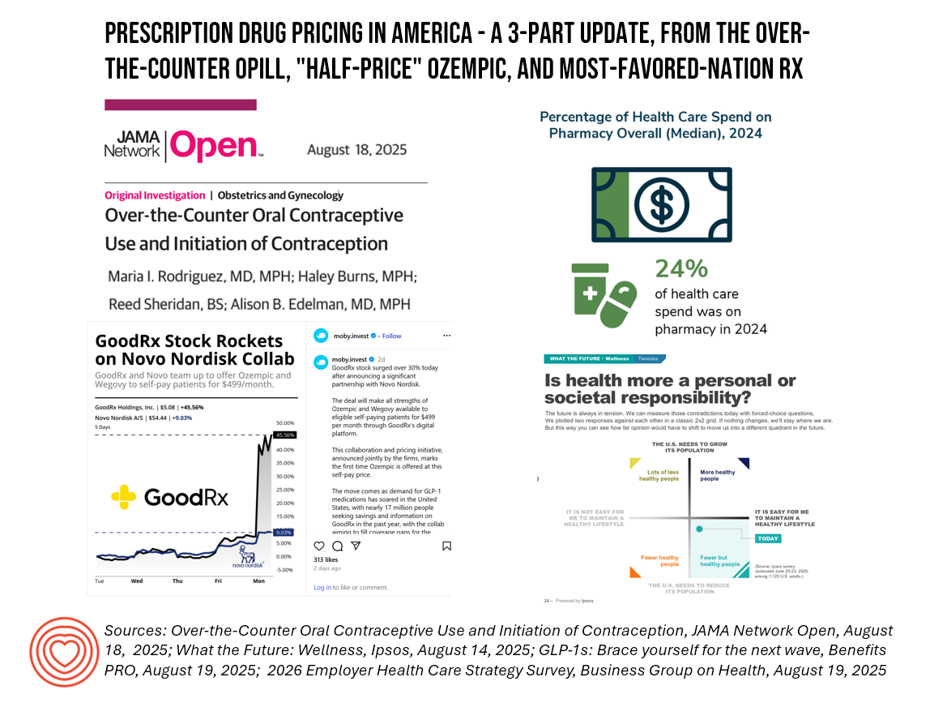
In this, Part 1 of a 3-part post, I will discuss research published this week in JAMA on the impact of contraceptive pills going over-the-counter (discussed previously here in Health Populi) along with proposed direct-to-consumer/-patient programs for GLP-1s and how the Trump Administration’s discussions for “Most Favored Nations” approach to drug pricing could re-shape the affordability and accessibility of medicines in America and in particular, for patients-as-consumers and the ultimate payors for prescription drugs. 
With the FDA’s approval of the first over-the-counter oral contraceptive pill in 2023, a new supply-channel was open to women seeking to prevent pregnancy: the OPill from Perrigo.
Researchers from the Oregon Health & Science University studied a sample of 986 women between 15 and 45 years of age who obtained these pills at pharmacies or online between April 2024 and February 2025. They had two key outcomes to measure:
- Women’s initiation of the contraception when not using any modern method, and,
- Women’s transition from a less-effective method to OPill use. (FYI, “less-effective” methods included condoms or forms of emergency contraception).

The graphic titled “Table 3” details the data which shows that the OTC contraception was obtained by many new users and people using less-effective methods. These observations support the finding that removing prescription requirements for contraceptive bills would expand access to the medicines, especially impactful for under-served populations like people uninsured and/or living in rural areas or those in OB-GYN shortage areas.

Among the women in the study, nearly 32% adopted use of the OPill who had not used any other contraceptive benefit. There was also a 41% increase among women who switched from less-effective methods of contraception to the OTC pill.
“Opill, the over-the-counter, progestin-only pill from drugmaker Perrigo, provides an option for obtaining oral contraceptives without needing to first see a health care provider. Allowing people to access the pill without a prescription was done in hopes of reducing barriers to access.” Sara Moniuszko wrote for CBS News on the JAMA research.
Stay tuned for Part 2 of this 3-part discussion in tomorrow’s Health Populi blog which will focus on Novo Nordisk’s 50% “discount” on Ozempic announced earlier this week — and how this collaboration with GoodRx is further re-shaping how consumers can access prescription drugs without an intermediary PBM.