There are many ways to measure the dysfunction of health care in the U.S.: we can point to relatively poor incomes relative to the rest of the developed world, given how much money is allocated to health care in America. The maternal mortality rate in the U.S. is unconscionably high, akin to some middle- and lower-income nations in the world. And medical debt is a uniquely American form of financial toxicity compared with other OECD nations where the concept is, well, foreign.
Even with these many failures, though, it’s important to put U.S. health care in a larger context: the health care industry can do what it can do to improve health care delivery, efficiency, patient engagement, and service design, for sure. But there’s a broader environmental context in which health care functions; consider public policy (across all levels from local to national to global), climate risks, and technology developments, just for a start.

As the annual AHIP 2025 conference kicks off on June 16th in Las Vegas, it’s a good time to consider that broader context for the health insurance and the overall health care ecosystem. As a member of the AHIP 2025 Advisory Board, I provided input into and guidance for this year’s conference with my particular focus on health policy, economics, innovative technology, and consumers as health citizens.
In my lead-up to AHIP 2024 last year, I deployed my go-to tools of scenario planning, resulting in four alternative futures for health care in the U.S. anticipating the 2024 U.S. elections and the post/long-COVID journey.

Let’s use that past as prologue or mental springboard for our AHIP 2025 lens, recalling the four futures shown here from that analysis:
- The Health Consumer as CEO of their care
- Retail Health for All
- One World, One Health, and,
- Fragmentation Meets Bureaucracy – where patients feel akin to castaways in a labyrinthine, un-friendly un-system.
The two uncertainties on which I chose to build the 2×2 matrix were,
- Public sector/government payment vs. private/commercial funding, and,
- Community ethos vs. individualistically-driven.
In constructing stories in scenario planning, we look to certainties (what we know we know), uncertainties (what we know we don’t know), and wild cards (the stuff that can happen that blow the assumptions up, forcing us to shifting our focus[es] and expectations).
For 2025, my spidey-senses tell me to re-visit last year’s uncertainties, considering the White House’s approach(es) to tariffs and Executive Orders, global political maneuvers (which can also impact trade as well as human capital, IP, and potential brain drain out of U.S. to more science-welcoming regimes), and environmental disasters that can dramatically shift the supply curves for agricultural output (think: fires or heat in produce-growing regions). Marry certain tariff regimes to environmental risks and a result can be a double-whammy on food systems, or immigration trends and public health challenges (say, the next pandemic).

For U.S. health care and AHIP 2025, I’ve updated some uncertainties that have significantly shifted in the past year, shown in the second chart. Of particular note and concern is the call-out from the 2025 Edelman Trust Barometer that this year embodies The Age of Grievance. There’s no greater evidence of that than the murder of UnitedHealthcare CEO Brian Thompson, an act that may have been motivated by antipathy toward the health care industry – specifically, health insurance, which is the core institution that AHIP serves.
Many of the uncertainties shown here will be addressed by various sessions and talks at AHIP 2025. And many of these forces overlap which suggests we collaborate on solutions across our ecosystem to deal with the really tough challenges our industry faces, in and beyond the health plan business.
Health Populi’s Hot Points: I’ll end with a riff on James Carville’s original, “it’s the economy, stupid,” related to voters’ votes. A few years later, (one of my mentors) Professor Uwe Reinhardt noted in Health Affairs that, “It’s the prices stupid” when it came to health care spending in the U.S. compared with other countries. Of course, it’s still the prices these days as we wrestle with approaches to managing the prices of prescription drugs while trying to assure innovation and U.S. excellence in life science research.
My mantra for AHIP 2025 and helping health care in America is now, “It’s the interconnections, stupid,” with due respect to all of us trying to deliver on the promise of health and care for all health citizens.
In response to his deep reading of The MAHA report, Dr. Neal Shah, wrote on his LinkedIn channel,
“I welcome this HUGE shift toward prevention. But, we can’t just rely on the government to fix healthcare. Everyone who stocks a pantry, writes a prescription, designs a school lunch, or codes a data dashboard, has an impact on the future of healthcare in America. Let’s all step up and do our part!”
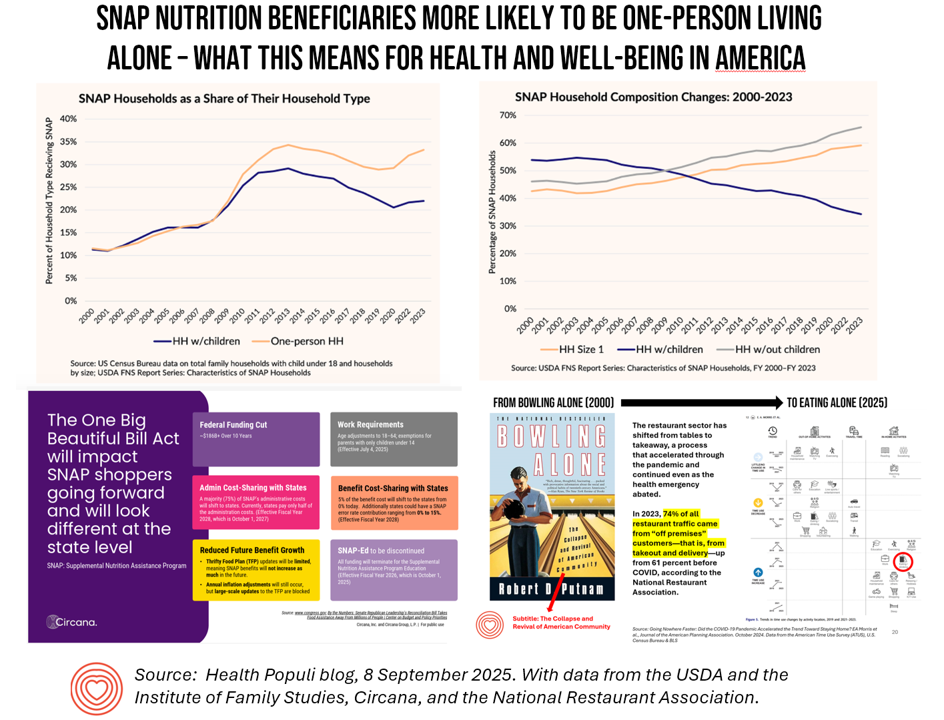
Dr. Shah is right, of course, to point out that our collaborations across industry segments in the health/care ecosystem and adjacent industries play roles in solving for America’s health care system deficiencies–but layer on top a major policy change. Think about health citizens’ access to health care due to cuts to Medicaid that then negatively impact the enabling technologies for access such Lyft and Uber. Similarly, cuts to SNAP benefits would negatively impact consumers’ connection with, say, Instacart, which has been an innovative connector between healthy food and medically-prescribed meals and patients.
Four of the largest Catholic health systems in the U.S. — Ascension, Providence, SSM Health, and Trinity Health — met on May 20th on Capitol Hill to share their concerns about the re-shaping of health policy in the U.S. and how various policy changes would negatively impact people for whom these health systems care, saying the policies would create “a polycrisis.” The Catholic Health Association published this statement on May 22nd, opposing H.R. 1, The One Big Beautiful Bill. “H.R. 1 would harm critical health and social safety-net programs that millions of Americans rely on to live with health, dignity, and security,” the CHA letter asserted.
There are many moving and interconnected pieces to solving for making (and nudging) people in America to be healthy (again), many of which are missing from or minimized in The MAHA Report. Connecting with these omitted areas will be crucial in addressing the root causes of un-well-being in the U.S. Just a few of these drivers of health beyond healthcare are,
- Financial wellbeing of individuals, families, and households (think jobs, wages, housing security which has been found to directly influence health status, including mental health).
- Respect for individuals’ data and the real-world evidence base that consumers – health citizens – could or would contribute were people to be assured privacy and security of their data, and respect for their individuality and consumer sovereign choices in a free society (see this new piece on the “Privacy-Compassion Trade-Off” to consider the concept of “emotional surveillance” and the kind of data that we might choose not to collect to benefit trust).
- Regulations on environmental hazards that the free market cannot and does not assure – which is why many of the regulations were put in place to begin with to enable health citizens to breathe in clean air and consume clean water, for example.
- Showing respect for other people who are different than one might be — for example, engaging in civil discourse, avoiding bullying in social media and other venues, and so on.

One area of collaboration that’s promising is working together to address data interoperability, which remains a barrier to improving health care for all. If you have ideas to share, the Centers for Medicare and Medicaid Services (CMS) within the Department of Health and Human Services has issued an RFI to ask for your ideas on interoperability. Check out Dr. Josh Mandel’s call-to-action here to be part of that collab and sharing.
This round for AHIP 2025 and the year in health care, I’m thinking interoperability and the Human OS (or human operating system and how we inter-relate and -operate with each other) – repeating the mantra,
If you want to go fast, go alone. If you want to go far, go together.