Feeling anxious? Can’t concentrate at work? Wake up drenched in sweat? Welcome to the overlooked and often maddening world of the perimenopause.
This transitional phase, in which symptoms of the menopause are experienced but periods haven’t yet stopped, was once dismissed as a hormonal blip. Now, it is increasingly recognised as an often unpleasant and disruptive stage of up to 10 years, during which the body and brain both undergo profound changes.
Mood swings, migraines, heart palpitations, urinary tract infections – the laundry list of symptoms can leave some people unable to recognise themselves. Thankfully, as our understanding of hormones grows, therapies are beginning to offer meaningful relief.
Yet there is no shortage of noise to wade through: social media overflows with recommendations for treatments, such as nutritional supplements or complex exercise regimes. So, what really works and what is simply a waste of time and money?
The answer comes down to how and why we experience perimenopause. During this period, oestrogen levels fluctuate erratically and, together with declines in progesterone and testosterone, affect everything from bone mass and muscle strength to cognition and cardiovascular risk.
And despite half the population going through this transition in their lives, its impact is wildly underestimated. “Menopause is a critical turning point in a woman’s life, physically, emotionally and socially,” says Cristina Del Toro Badessa, a physician and hormonal health expert based in Atlanta, Georgia. “[But] many women are part of the ‘sandwich generation’, caring for both children and ageing parents. Their own well-being is often overlooked.”
These symptoms are more than just a personal hardship; they can have wide-ranging societal impacts. A survey by UK charity Wellbeing of Women found that 1 in 4 women have considered leaving their jobs because of menopausal symptoms. In the US, a 2025 study estimated the toll of menopause costs the economy $1.8 billion each year due to reduced working hours or early retirement.

Many of those dealing with perimenopause symptoms take HRT
Elena Popova/Getty Images
When it comes to solutions, hormone replacement therapy (HRT) is the first-line treatment for anyone over 40, according to the UK’s National Institute of Health and Care Excellence (NICE). Yet despite its effectiveness, uptake remains patchy, and its use has plummeted in the US over the past 25 years. This is in part because of lingering fears over side effects brought to light in two studies. In 2002, a major trial of HRT was stopped after early results linked it to an increased risk of breast cancer, heart attacks and stroke. A second study in 2003 estimated that HRT was responsible for 20,000 cases of breast cancer in the past decade.
While the findings from these trials weren’t incorrect, they were limited in several important ways and their results were misinterpreted in the media. For example, they focused on women over 60 – subsequent trials have shown how a woman’s age when starting HRT affects the risk of breast cancer, as does how long she takes it. For instance, five years after stopping HRT there is no increased breast cancer risk for women who took HRT for less than five years.
Context also matters. According to the British Menopause Society, for women taking combined HRT (both oestrogen and progestogen) for up to 14 years, there are 10 additional breast cancer diagnoses per 1000 women aged 50 to 59. However, it says this “small risk” should be weighed against the significant decrease in risk of endometrial cancer that HRT provides. It also points out that this is similar to other lifestyle factors: obesity causes an extra 10 additional breast cancer diagnoses per 1000 women aged 50 to 59. Similarly, drinking 4 to 6 units of alcohol per day increases the number of cases by eight. In other words, HRT slightly increases the risk of being diagnosed with breast cancer, but not dramatically, and no more than several other lifestyle factors.
The benefits of HRT
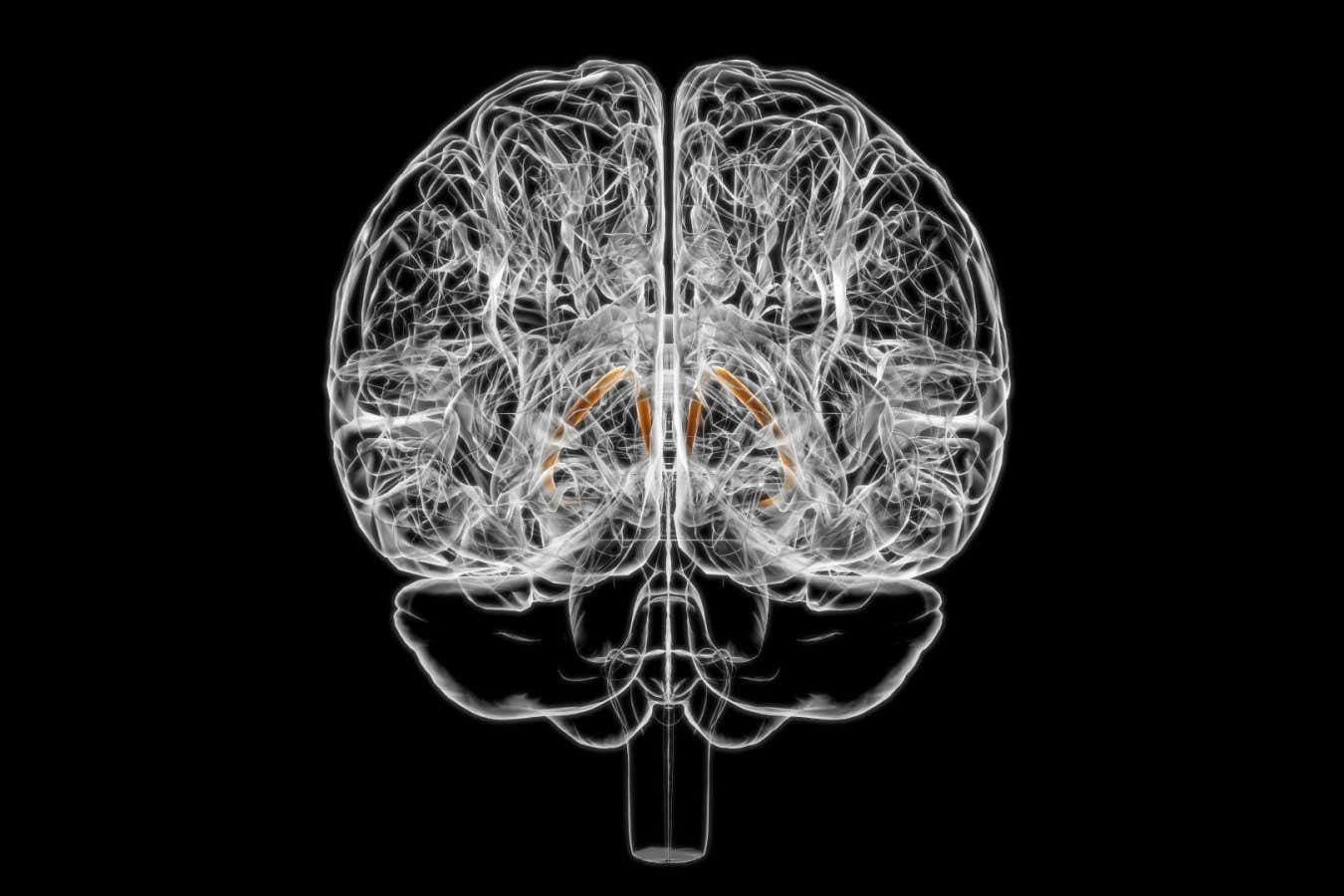
And there are benefits, too. HRT reduces the risk of cardiovascular disease and decreases bone fractures. There is also early evidence that oestrogen is vital for helping the brain regulate glucose metabolism – the loss of oestrogen during perimenopause and the subsequent effect on glucose metabolism potentially explains perimenopausal fatigue and forgetfulness. Research by Roberta Brinton at the University of Arizona and her colleagues suggests that HRT may also provide some protection against Alzheimer’s – although this is still a fairly controversial idea.
“All menopause guidelines state that hormone replacement therapy is the most evidence-based treatment for perimenopausal symptoms,” says Louise Newson, a physician and member of the UK government’s Menopause Taskforce.
Still, HRT isn’t for everyone. Some women have additional risk factors that rule it out, such as those with lupus or a history of blood clots, while others are reluctant to accept the associated risks. That is why researchers such as Karyn Frick at the University of Wisconsin-Milwaukee are investigating highly selective oestrogen receptor drugs. Unlike current HRT, which activates a broad spectrum of oestrogen receptors, these drugs target only those that are linked with protective effects, such as inhibiting breast and ovarian cancer cell proliferation. Initial studies suggest this approach could prove more effective than existing treatments.
NICE also recommends cognitive behavioural therapy as the other frontline treatment for perimenopause. Clinical trials have shown that CBT techniques can reduce hot flushes and night sweats.
Speaking of hot flushes, drug developers are on the case. In 2023, the US Food and Drug Association approved fezolinetant, the first non-hormonal drug developed for this symptom. It works by blocking NK3 receptors in the brain that regulate the body’s internal thermostat, which are hyperactive in a low-oestrogen environment. “This drug works quickly and effectively,” says Alyssa Dweck, consultant gynaecologist and chief medical officer at US-based company Bonafide Health, which specialises in products to relieve menopause symptoms. The downside is that it is expensive, often lacks insurance coverage in the US and requires regular liver monitoring due to potential side effects.
A better option may turn out to be a related drug, elinzanetant, which was approved by the UK’s Medicines and Healthcare products Regulatory Agency in July. It targets NK1 receptors alongside NK3, and in early trials it not only reduced moderate to severe hot flushes, but also cut sleep disturbances and showed no incidences of liver toxicity.
Should I eat more protein during perimenopause?
Of course, medicine is just part of the solution. Dietary tweaks can also be effective. Many influencers swear by “eating more protein”, and when it comes to perimenopause, they may be on to something. While most people meet their protein needs through a balanced diet, hormonal changes during perimenopause can feel like they are working against you, causing accelerated bone and muscle loss. And despite this, many women gain weight for reasons that are unclear.
Arthur Conigrave at the University of Sydney thinks the answer lies in a mismatch between the body’s protein needs and intake. In 2022, he and his colleagues provided evidence that as protein in muscle breaks down, the brain ramps up appetite in an attempt to restore protein balance. But unless your diet is adjusted to increase the proportion of protein, people just eat more food overall, leading to weight gain.
Conigrave’s team suggests that during perimenopause, women may need to increase daily protein by about 0.1 gram to 0.2g per kilogram of bodyweight. For someone weighing 70 kg (around 155 pounds) that is an extra 7g to 14g a day, about what is found in a large egg or a cup of edamame.
Do any perimenopause-targeting supplements actually work?
Despite the hype, evidence is patchy for supplements as a treatment for perimenopause. A 2021 review found only one extract – Cimicifuga racemosa, or black cohosh – had strong supporting evidence of its efficacy, with studies suggesting it may reduce anxiety, irritability and heart palpitations. This could potentially work by increasing levels of serotonin, but results vary and safety hasn’t been fully established. Vitamin B6, which has a role in maintaining the nervous system, can also reduce hot flushes and protect against cognitive dysfunction, while ensuring recommended levels of vitamin D can prevent low mood and boost the immune system. Still, these dietary additions won’t necessarily be transformative.

Lifting weights during perimenopause can improve bone density – which can be compromised through declining oestrogen levels
Elena Popova/Getty Images
“Some vitamins and supplements may improve some symptoms, but they will not replace the missing hormones and will not have the long-term health benefits that HRT does,” says Newson. Some studies suggest, for instance, that HRT reduces long-term risk of heart disease and diabetes.
There is also growing interest in the microbiome and how it changes during menopause. A recent review of all the current evidence demonstrated that probiotics had a positive effect on perimenopausal bone health, hot flushes, psychological symptoms and vaginal dryness – though many studies had a high risk of bias due to flaws in design, conduct or analysis, so more rigorous research is needed.
Should I lift weights or go for a run?
Finally, there is the question of the best exercise routine to counter the effects of perimenopause: should you pound the pavement or concentrate on strength training? A review of studies from 2015 to 2022 confirmed that weight workouts during perimenopause improve strength, bone density and metabolic health, but concluded that it was still unclear whether this kind of regime outperforms other types of exercise.
As for the rest of the “advice” on social media? Proceed with caution. While regulators are clamping down on spurious claims, there is still a touch of the Wild West in this space. And until more focus – and funding – is directed towards understanding conditions primarily affecting women, that is unlikely to change any time soon.
Topics: